What Should We Do About Achilles Tendon Pain ?
Overview
 Achilles tendinitis, also known as Achilles tendonitis, is inflammation of the Achilles tendon. The Achilles tendon connects your calf muscles to the back of your heel bone. It allows extension of your foot downward, away from your body, which lets your heel lift off the ground as you move forward when walking. Every time you take a step you rely on your Achilles tendon.
Achilles tendinitis, also known as Achilles tendonitis, is inflammation of the Achilles tendon. The Achilles tendon connects your calf muscles to the back of your heel bone. It allows extension of your foot downward, away from your body, which lets your heel lift off the ground as you move forward when walking. Every time you take a step you rely on your Achilles tendon.
Causes
When you place a large amount of stress on your Achilles tendon too quickly, it can become inflamed from tiny tears that occur during the activity. Achilles tendonitis is often a result of overtraining, or doing too much too soon. Excessive hill running can contribute to it. Flattening of the arch of your foot can place you at increased risk of developing Achilles tendonitis because of the extra stress placed on your Achilles tendon when walking or running.
Symptoms
The most common site of Achilles Tendonitis is at the heel to 4 inches above the heel. The diagnosis of this problem is made when the following signs are present. Pain in the Achilles tendon with up and down movement of the foot at the ankle. Pain in the Achilles tendon when you squeeze the tendon from side to side. If you are unable to move the foot either up or down, or you have intense pain when trying to walk, you may have a tear of the Achilles tendon, and you should see a doctor immediately. Also if you have severe pain in the calf, with or without discolorations of the skin, you may have a blood clot, and this is a medical emergency; see a doctor immediately. If you do not fall into either of these categories then try the following suggestions.
Diagnosis
A podiatrist can usually make the diagnosis by clinical history and physical examination alone. Pain with touching or stretching the tendon is typical. There may also be a visible swelling to the tendon. The patient frequently has difficulty plantarflexing (pushing down the ball of the foot and toes, like one would press on a gas pedal), particularly against resistance. In most cases X-rays don't show much, as they tend to show bone more than soft tissues. But X-rays may show associated degeneration of the heel bone that is common with Achilles Tendon problems. For example, heel spurs, calcification within the tendon, avulsion fractures, periostitis (a bruising of the outer covering of the bone) may all be seen on X-ray. In cases where we are uncertain as to the extent of the damage to the tendon, though, an MRI scan may be necessary, which images the soft tissues better than X-rays. When the tendon is simply inflamed and not severely damaged, the problem may or may not be visible on MRI. It depends upon the severity of the condition.
Nonsurgical Treatment
Treatment options might include anti-inflammatory medication such as ibuprofen which might help with acute achilles inflammation and pain but has not been proven to be beneficial long term and may even inhibit healing. If the injury is severe then a plaster cast might be applied to immobilize the tendon. Use of electrotherapy such as ultrasound treatment, laser therapy and extracorporeal shock wave therapy (ESWT) may be beneficial in reducing pain and encouraging healing. Applying sports massage techniques can mobilze the tissues or the tendon itself and help stretch the calf muscles. Some might give a steroid injection however an injection directly into the tendon is not recommended. Some specialists believe this can increase the risk of a total rupture of the tendon in future. One of the most effective forms of treatment for achilles tendonitis is a full rehabilitation program consisting of eccentric strengthening exercises. There is now considerable evidence suggesting the effectiveness of slow eccentric rehabilitation exercises for curing achilles tendon pain.

Surgical Treatment
Histological and biological studies on tendon healing have made it possible to envisage surgical repair using a percutaneous approach, with the following objectives, a minimal, and not very aggressive, operation, which is quick and easy and within the capabilities of all surgeons, the shortest hospitalisation period possible, above all, early and effective re-education, providing a satisfactory result both in terms of solidity and the comfort of the patient. The percutaneous tenosynthesis TENOLIG combines stability, reliability, patient comfort and lower overall social and professional costs for this type of lesion.
Prevention
Do strengthening and stretching exercises to keep calf muscles strong and flexible. Keep your hamstring muscles flexible by stretching. Warm up and stretch adequately before participating in any sports. Always increase the intensity and duration of training gradually. Do not continue an exercise if you experience pain over the tendon. Wear properly fitted running and other sports shoes, including properly fitted arch supports if your feet roll inwards excessively (over-pronate).
 Achilles tendinitis, also known as Achilles tendonitis, is inflammation of the Achilles tendon. The Achilles tendon connects your calf muscles to the back of your heel bone. It allows extension of your foot downward, away from your body, which lets your heel lift off the ground as you move forward when walking. Every time you take a step you rely on your Achilles tendon.
Achilles tendinitis, also known as Achilles tendonitis, is inflammation of the Achilles tendon. The Achilles tendon connects your calf muscles to the back of your heel bone. It allows extension of your foot downward, away from your body, which lets your heel lift off the ground as you move forward when walking. Every time you take a step you rely on your Achilles tendon.
Causes
When you place a large amount of stress on your Achilles tendon too quickly, it can become inflamed from tiny tears that occur during the activity. Achilles tendonitis is often a result of overtraining, or doing too much too soon. Excessive hill running can contribute to it. Flattening of the arch of your foot can place you at increased risk of developing Achilles tendonitis because of the extra stress placed on your Achilles tendon when walking or running.
Symptoms
The most common site of Achilles Tendonitis is at the heel to 4 inches above the heel. The diagnosis of this problem is made when the following signs are present. Pain in the Achilles tendon with up and down movement of the foot at the ankle. Pain in the Achilles tendon when you squeeze the tendon from side to side. If you are unable to move the foot either up or down, or you have intense pain when trying to walk, you may have a tear of the Achilles tendon, and you should see a doctor immediately. Also if you have severe pain in the calf, with or without discolorations of the skin, you may have a blood clot, and this is a medical emergency; see a doctor immediately. If you do not fall into either of these categories then try the following suggestions.
Diagnosis
A podiatrist can usually make the diagnosis by clinical history and physical examination alone. Pain with touching or stretching the tendon is typical. There may also be a visible swelling to the tendon. The patient frequently has difficulty plantarflexing (pushing down the ball of the foot and toes, like one would press on a gas pedal), particularly against resistance. In most cases X-rays don't show much, as they tend to show bone more than soft tissues. But X-rays may show associated degeneration of the heel bone that is common with Achilles Tendon problems. For example, heel spurs, calcification within the tendon, avulsion fractures, periostitis (a bruising of the outer covering of the bone) may all be seen on X-ray. In cases where we are uncertain as to the extent of the damage to the tendon, though, an MRI scan may be necessary, which images the soft tissues better than X-rays. When the tendon is simply inflamed and not severely damaged, the problem may or may not be visible on MRI. It depends upon the severity of the condition.
Nonsurgical Treatment
Treatment options might include anti-inflammatory medication such as ibuprofen which might help with acute achilles inflammation and pain but has not been proven to be beneficial long term and may even inhibit healing. If the injury is severe then a plaster cast might be applied to immobilize the tendon. Use of electrotherapy such as ultrasound treatment, laser therapy and extracorporeal shock wave therapy (ESWT) may be beneficial in reducing pain and encouraging healing. Applying sports massage techniques can mobilze the tissues or the tendon itself and help stretch the calf muscles. Some might give a steroid injection however an injection directly into the tendon is not recommended. Some specialists believe this can increase the risk of a total rupture of the tendon in future. One of the most effective forms of treatment for achilles tendonitis is a full rehabilitation program consisting of eccentric strengthening exercises. There is now considerable evidence suggesting the effectiveness of slow eccentric rehabilitation exercises for curing achilles tendon pain.

Surgical Treatment
Histological and biological studies on tendon healing have made it possible to envisage surgical repair using a percutaneous approach, with the following objectives, a minimal, and not very aggressive, operation, which is quick and easy and within the capabilities of all surgeons, the shortest hospitalisation period possible, above all, early and effective re-education, providing a satisfactory result both in terms of solidity and the comfort of the patient. The percutaneous tenosynthesis TENOLIG combines stability, reliability, patient comfort and lower overall social and professional costs for this type of lesion.
Prevention
Do strengthening and stretching exercises to keep calf muscles strong and flexible. Keep your hamstring muscles flexible by stretching. Warm up and stretch adequately before participating in any sports. Always increase the intensity and duration of training gradually. Do not continue an exercise if you experience pain over the tendon. Wear properly fitted running and other sports shoes, including properly fitted arch supports if your feet roll inwards excessively (over-pronate).
Pes Planus?
Overview

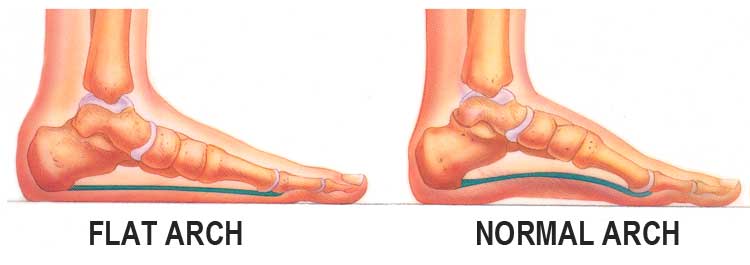
?Life begins at 40,? goes an old quote, ?and so do fallen arches.? It?s time to toss that negative idea out the window and get the real facts on fallen arches and what you can do about them. We have all seen what our footprints look like as we walked across sand or left a water trail after getting out of the bathtub. The narrow part of the footprint is where your natural arch exists. What gives you that arch are tendons that pull together to create an upward curve. When your tendons are not properly pulling together, you start to lose that natural arch. This condition is known as flat foot or fallen arch.
Causes
Flat feet are a common condition. In infants and toddlers, the arch is not developed and flat feet are normal. The arch develops in childhood. By adulthood, most people have developed normal arches. When flat feet persist, most are considered variations of normal. Most feet are flexible and an arch appears when the person stands on his or her toes. Stiff, inflexible, or painful flat feet may be associated with other conditions and require attention. Painful flat feet in children may be caused by a condition called tarsal coalition. In tarsal coalition, two or more of the bones in the foot fuse together. This limits motion and often leads to a flat foot. Most flat feet do not cause pain or other problems. Flat feet may be associated with pronation, in which the ankle bones lean inward toward the center line. When the shoes of children who pronate are placed side by side, they will lean toward each other (after they have been worn long enough for the foot position to remodel their sole). Foot pain, ankle pain, or lower leg pain (especially in children) may be a result of flat feet and should be evaluated by a health care provider. Adults can develop a flat foot when they are 60 - 70 years old. This type of flat foot is usually on one side.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
There are a few simple ways to assess your foot type, and most include making an imprint of your footprint. The classic way is to stand on a hard floor surface with wet feet to make a wet foot print. Look at the narrowest part of your footprint, which should be between your heel and ball of your foot. If the print of your foot in this part is less than 10% of the width of the widest part then you are likely to have high arches. more than 10% but less than 25% then your foot profile is probably normal, more than 25% or even the widest part, then you have flat feet.
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
Donning a first-rate pair of arch supports, therapeutic socks and proper footwear before heading out to enjoy hours of holiday fun is one option to consider. Your podiatrist can help you find just the right ones. Once you have them on, they?ll help ease the amount of pressure being put on your body and keep the blood flowing in the right direction. While you?re standing in line, consider doing a bit of exercise as well. We?re not talking about channeling your inner Jack LaLanne here. Otherwise, you might attract the attention of the mall security guards. Simple ankle rotations and walking in place may help to reduce edema and give your flat feet a bit of a break. If you happen to be in a shopping mall or center where foot massages are available, take advantage of them periodically. They are likely to make you feel better and it?s a great excuse to carve out a few quiet moments for yourself. If you can?t visit a professional, tuck a personal foot massager into your purse. That way, you can lightly massage your own feet during the car ride home. Lastly, there are certain foods and nutritional supplements available that may reduce edema caused by standing on flat feet for hours at a time. The list includes potassium rich foods like raisins, bananas, baby carrots, nuts and yogurt. So, you may want to pack a snack for those trips to the mall or hit the food court before you hit the stores.

?Life begins at 40,? goes an old quote, ?and so do fallen arches.? It?s time to toss that negative idea out the window and get the real facts on fallen arches and what you can do about them. We have all seen what our footprints look like as we walked across sand or left a water trail after getting out of the bathtub. The narrow part of the footprint is where your natural arch exists. What gives you that arch are tendons that pull together to create an upward curve. When your tendons are not properly pulling together, you start to lose that natural arch. This condition is known as flat foot or fallen arch.
Causes
Flat feet are a common condition. In infants and toddlers, the arch is not developed and flat feet are normal. The arch develops in childhood. By adulthood, most people have developed normal arches. When flat feet persist, most are considered variations of normal. Most feet are flexible and an arch appears when the person stands on his or her toes. Stiff, inflexible, or painful flat feet may be associated with other conditions and require attention. Painful flat feet in children may be caused by a condition called tarsal coalition. In tarsal coalition, two or more of the bones in the foot fuse together. This limits motion and often leads to a flat foot. Most flat feet do not cause pain or other problems. Flat feet may be associated with pronation, in which the ankle bones lean inward toward the center line. When the shoes of children who pronate are placed side by side, they will lean toward each other (after they have been worn long enough for the foot position to remodel their sole). Foot pain, ankle pain, or lower leg pain (especially in children) may be a result of flat feet and should be evaluated by a health care provider. Adults can develop a flat foot when they are 60 - 70 years old. This type of flat foot is usually on one side.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
There are a few simple ways to assess your foot type, and most include making an imprint of your footprint. The classic way is to stand on a hard floor surface with wet feet to make a wet foot print. Look at the narrowest part of your footprint, which should be between your heel and ball of your foot. If the print of your foot in this part is less than 10% of the width of the widest part then you are likely to have high arches. more than 10% but less than 25% then your foot profile is probably normal, more than 25% or even the widest part, then you have flat feet.
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
Donning a first-rate pair of arch supports, therapeutic socks and proper footwear before heading out to enjoy hours of holiday fun is one option to consider. Your podiatrist can help you find just the right ones. Once you have them on, they?ll help ease the amount of pressure being put on your body and keep the blood flowing in the right direction. While you?re standing in line, consider doing a bit of exercise as well. We?re not talking about channeling your inner Jack LaLanne here. Otherwise, you might attract the attention of the mall security guards. Simple ankle rotations and walking in place may help to reduce edema and give your flat feet a bit of a break. If you happen to be in a shopping mall or center where foot massages are available, take advantage of them periodically. They are likely to make you feel better and it?s a great excuse to carve out a few quiet moments for yourself. If you can?t visit a professional, tuck a personal foot massager into your purse. That way, you can lightly massage your own feet during the car ride home. Lastly, there are certain foods and nutritional supplements available that may reduce edema caused by standing on flat feet for hours at a time. The list includes potassium rich foods like raisins, bananas, baby carrots, nuts and yogurt. So, you may want to pack a snack for those trips to the mall or hit the food court before you hit the stores.
Achilles Tendonitis Painfulness Treatments And Causes
Overview
 You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
Causes
The cause of paratenonitis is not well understood although there is a correlation with a recent increase in the intensity of running or jumping workouts. It can be associated with repetitive activities which overload the tendon structure, postural problems such as flatfoot or high-arched foot, or footwear and training issues such as running on uneven or excessively hard ground or running on slanted surfaces. Tendinosis is also associated with the aging process.
Symptoms
Pain in the back of the heel that can be a shooting pain, burning pain or even an intense piercing pain. Swelling, tenderness and warmth over the Achilles tendon especially at the insertion of the tendon to the calcaneous, which may even extend into the muscle of the calf. Difficulty walking, sometimes the pain makes walking impossible. Pain that is aggravated by activities that repeatedly stress the tendon, causing inflammation or pain that occurs in the first few steps of the morning or after sitting down for extended periods of time which gets better with mild activity. It is important to note though that achilles tendinosis can develop gradually without a history of trauma.
Diagnosis
Studies such as x-rays and MRIs are not usually needed to make the diagnosis of tendonitis. While they are not needed for diagnosis of tendonitis, x-rays may be performed to ensure there is no other problem, such as a fracture, that could be causing the symptoms of pain and swelling. X-rays may show evidence of swelling around the tendon. MRIs are also good tests identify swelling, and will show evidence of tendonitis. However, these tests are not usually needed to confirm the diagnosis; MRIs are usually only performed if there is a suspicion of another problem that could be causing the symptoms. Once the diagnosis of tendonitis is confirmed, the next step is to proceed with appropriate treatment. Treatment depends on the specific type of tendonitis. Once the specific diagnosis is confirmed, the appropriate treatment of tendonitis can be initiated.
Nonsurgical Treatment
Relieving the stress is the first course of action. Treatment involves ice therapy and activity modification to reduce inflamation. Active stretching and strengthening exercises will assist rehabilitation of the gastrocnemius-soleus complex. When placed in a heeled shoe, the patient will immediately notice a difference, compared to flat ground. It is recommended that the patient be fitted with proper shoes & orthotics to control pronation and maintain proper alignment, relieving the stress on the achilles tendon. Tightness in the tendon itself can be helped by an extra heel lift added to the orthotics. The patient can expect a slow recovery over a period of months.

Surgical Treatment
Surgery is considered the last resort. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon. Rehabilitation, including stretching and strength exercises, is started soon after the surgery. In most cases, normal activities can be resumed after about 10 weeks. Return to competitive sport for some people may be delayed for about three to six months.
Prevention
Warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you?re overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
 You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
You?re a prime candidate for acquiring Achilles Tendonitis if you?re a runner or some other kind of athlete requiring heavy use of your calves and their attached tendons. Then again, -anybody- can get tendonitis of the Achilles tendons. All for very predictable reasons. Perhaps you have Achilles Tendon pain from cycling. Or standing at work. Or walking around a lot. Anything we do on our feet uses our lower leg structures, and the Achilles tendon bears LOTS of torque, force, load, etc. The physical dynamic called Tendonitis can show up anywhere. On the Achilles Tendon is as good a place as any. Repetitive strain injury can show up anywhere in the body that there is repetitive strain. It's an obvious statement, but worth paying attention to.
Causes
The cause of paratenonitis is not well understood although there is a correlation with a recent increase in the intensity of running or jumping workouts. It can be associated with repetitive activities which overload the tendon structure, postural problems such as flatfoot or high-arched foot, or footwear and training issues such as running on uneven or excessively hard ground or running on slanted surfaces. Tendinosis is also associated with the aging process.
Symptoms
Pain in the back of the heel that can be a shooting pain, burning pain or even an intense piercing pain. Swelling, tenderness and warmth over the Achilles tendon especially at the insertion of the tendon to the calcaneous, which may even extend into the muscle of the calf. Difficulty walking, sometimes the pain makes walking impossible. Pain that is aggravated by activities that repeatedly stress the tendon, causing inflammation or pain that occurs in the first few steps of the morning or after sitting down for extended periods of time which gets better with mild activity. It is important to note though that achilles tendinosis can develop gradually without a history of trauma.
Diagnosis
Studies such as x-rays and MRIs are not usually needed to make the diagnosis of tendonitis. While they are not needed for diagnosis of tendonitis, x-rays may be performed to ensure there is no other problem, such as a fracture, that could be causing the symptoms of pain and swelling. X-rays may show evidence of swelling around the tendon. MRIs are also good tests identify swelling, and will show evidence of tendonitis. However, these tests are not usually needed to confirm the diagnosis; MRIs are usually only performed if there is a suspicion of another problem that could be causing the symptoms. Once the diagnosis of tendonitis is confirmed, the next step is to proceed with appropriate treatment. Treatment depends on the specific type of tendonitis. Once the specific diagnosis is confirmed, the appropriate treatment of tendonitis can be initiated.
Nonsurgical Treatment
Relieving the stress is the first course of action. Treatment involves ice therapy and activity modification to reduce inflamation. Active stretching and strengthening exercises will assist rehabilitation of the gastrocnemius-soleus complex. When placed in a heeled shoe, the patient will immediately notice a difference, compared to flat ground. It is recommended that the patient be fitted with proper shoes & orthotics to control pronation and maintain proper alignment, relieving the stress on the achilles tendon. Tightness in the tendon itself can be helped by an extra heel lift added to the orthotics. The patient can expect a slow recovery over a period of months.

Surgical Treatment
Surgery is considered the last resort. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon. Rehabilitation, including stretching and strength exercises, is started soon after the surgery. In most cases, normal activities can be resumed after about 10 weeks. Return to competitive sport for some people may be delayed for about three to six months.
Prevention
Warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you?re overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
Do I Have Fallen Arches??
Overview

Flat feet and fallen arches refer to the same thing. It's a downward sagging of the inside edge of the foot during standing or walking. The front-to-back arches (called the longitudinal arches) are natural curves along the bottoms of both feet that are supported by muscles and ligaments. When these muscles and ligaments give way, the arches sag with each step. When the arches sag, your weight is shifted toward your big toes.
Causes
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time. Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
Non Surgical Treatment
The treatment your podiatrist recommends will depend upon the trouble and pain you?re experiencing. Custom shoe inserts (orthotics) are most often recommended and are quite effective. Stretching exercises to loosen and strengthen the supporting tendons may also be recommended. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Your foot and ankle surgeon may recommend changes in your footwear.
Surgical Treatment
Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

Flat feet and fallen arches refer to the same thing. It's a downward sagging of the inside edge of the foot during standing or walking. The front-to-back arches (called the longitudinal arches) are natural curves along the bottoms of both feet that are supported by muscles and ligaments. When these muscles and ligaments give way, the arches sag with each step. When the arches sag, your weight is shifted toward your big toes.
Causes
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time. Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
Non Surgical Treatment
The treatment your podiatrist recommends will depend upon the trouble and pain you?re experiencing. Custom shoe inserts (orthotics) are most often recommended and are quite effective. Stretching exercises to loosen and strengthen the supporting tendons may also be recommended. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Your foot and ankle surgeon may recommend changes in your footwear.
Surgical Treatment
Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Does Pain In The Arches Need Surgery ?
Overview
The arch of the foot is formed by the tarsal and metatarsal bones and is strengthened by ligaments and tendons that enable the foot to correctly support the weight of the body. The underside of the foot is made up of four layers of muscle tissue as well as a length of thick connective tissue called the plantar fascia, which supports the arch. If the surrounding muscles weaken, the plantar fascia will drop and the arch will collapse. If the arch collapses, the whole foot touches the ground, which is known as pes planus or flat feet. Flat feet affect about 15 per cent of Britons. Although usually genetic, the condition may be exacerbated or triggered by poorly fitted shoes or conditions such as arthritis and pregnancy, when sudden changes in shape and weight can alter the body's centre of gravity leading to a weakening of the arches.

Causes
Over-stretching or tearing the arch pad causes the dull ache that is associated with arch pain. Pain is most keenly felt when weight is put onto the foot, or when pushing off the foot into the next stride. The pain of foot arch strain can be particularly acute after sitting for a long time, or when getting up in the morning. Those most susceptible to the condition are people with very high, rigid arches. The injury is also common in middle-aged people who have been inactive for a long period of time before suddenly increasing their physical activity. The injury is particularly common in runners and joggers.
Symptoms
Persistant pain and selling under the ball of the foot and extending towards the toes (most commonly the 2nd). Some swelling may be disable on the top of the foot along with redness. Often a sensation of 'walking on the bones for the foot' will be described, and there is a positive Lachman's test. Often a tear will result in the toes splaying (daylight sign) and clawing.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
There are many different causes of and treatments for flat foot. The most important part of treatment is determining the exact flat foot type on an individual basis, and doing so early on. The main objective is to become educated on the potential problems, so that you can stop them before they start. Conservative treatment is often successful if initiated early. The old adage "a stitch in time saves nine" definitely applies to the human body, hopefully more figuratively than literally. Do not ignore what your common sense and your body are telling you. Yes, you can live without an arch, but never neglect a symptomatic foot. If you neglect your feet, they will make you pay with every literal step you take.

Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
Stretch and strengthen important muscles in your feet, ankles and legs in order to guard against future strain. Make sure to acquire suitable arch supports and inserts if necessary, and that your shoes are shock absorbent and in good condition. Wearing tattered shoes provides no protection, and runners should replace their footwear before exceeding 500 miles of usage. Athletes new to arch supports should gradually build their training routine, allowing their feet to become accustomed to a new stance.
Stretching Exercises
Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards. Push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee. Hold the stretch for 15 to 30 seconds and repeat with the opposite leg. Repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
The arch of the foot is formed by the tarsal and metatarsal bones and is strengthened by ligaments and tendons that enable the foot to correctly support the weight of the body. The underside of the foot is made up of four layers of muscle tissue as well as a length of thick connective tissue called the plantar fascia, which supports the arch. If the surrounding muscles weaken, the plantar fascia will drop and the arch will collapse. If the arch collapses, the whole foot touches the ground, which is known as pes planus or flat feet. Flat feet affect about 15 per cent of Britons. Although usually genetic, the condition may be exacerbated or triggered by poorly fitted shoes or conditions such as arthritis and pregnancy, when sudden changes in shape and weight can alter the body's centre of gravity leading to a weakening of the arches.
Causes
Over-stretching or tearing the arch pad causes the dull ache that is associated with arch pain. Pain is most keenly felt when weight is put onto the foot, or when pushing off the foot into the next stride. The pain of foot arch strain can be particularly acute after sitting for a long time, or when getting up in the morning. Those most susceptible to the condition are people with very high, rigid arches. The injury is also common in middle-aged people who have been inactive for a long period of time before suddenly increasing their physical activity. The injury is particularly common in runners and joggers.
Symptoms
Persistant pain and selling under the ball of the foot and extending towards the toes (most commonly the 2nd). Some swelling may be disable on the top of the foot along with redness. Often a sensation of 'walking on the bones for the foot' will be described, and there is a positive Lachman's test. Often a tear will result in the toes splaying (daylight sign) and clawing.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
There are many different causes of and treatments for flat foot. The most important part of treatment is determining the exact flat foot type on an individual basis, and doing so early on. The main objective is to become educated on the potential problems, so that you can stop them before they start. Conservative treatment is often successful if initiated early. The old adage "a stitch in time saves nine" definitely applies to the human body, hopefully more figuratively than literally. Do not ignore what your common sense and your body are telling you. Yes, you can live without an arch, but never neglect a symptomatic foot. If you neglect your feet, they will make you pay with every literal step you take.

Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
Stretch and strengthen important muscles in your feet, ankles and legs in order to guard against future strain. Make sure to acquire suitable arch supports and inserts if necessary, and that your shoes are shock absorbent and in good condition. Wearing tattered shoes provides no protection, and runners should replace their footwear before exceeding 500 miles of usage. Athletes new to arch supports should gradually build their training routine, allowing their feet to become accustomed to a new stance.
Stretching Exercises
Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards. Push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee. Hold the stretch for 15 to 30 seconds and repeat with the opposite leg. Repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Arch Pain Causes Symptoms And Treatments
Overview
Flexible flatfeet are considered normal in young children because babies are not born with a normal arch. The arch may not form fully until sometime between ages 7 and 10. Even in adulthood, 15% to 25% of people have flexible flatfeet. Most of these people never develop symptoms. In many adults who have had flexible flatfeet since childhood, the missing arch is an inherited condition related to a general looseness of ligaments. These people usually have extremely flexible, very mobile joints throughout the body, not only in the feet. Flatfeet also can develop during adulthood. Causes include joint disease, such as rheumatoid arthritis, and disorders of nerve function (neuropathy).

Causes
There are a number of other medical conditions that can cause foot arch pain such as diabetes, arthritis and obesity. These can affect the position and strength of the bones, muscles, ligaments and tendons, leading to bottom of foot pain. It sounds simple but footwear plays an important role in how our feet feel. Foot arch pain is commonly caused by ill-fitting shoes, especially ones with little arch support or that are too tight. Footwear is particularly important if you are going to be spending long periods on your feet or for sporting activities such as running. Shoes should be supportive, comfortable, cushioned, provide the appropriate level of arch support and be the correct width.
Symptoms
Pain in arch of foot is really the only symptom of this condition. It is unlikely to see any swelling or bruising and instead there will be a deep tender spot near the heel. Occasionally the pain may radiate further down the foot. With this condition, pain will usually be felt first thing in the morning or after periods of sitting. This is because the plantar fascia tightens and shortens slightly when there is no weight on it and by standing on it it suddenly stretches and becomes painful. After a few steps it starts to loosen off and the pain may subside. If this is the same pattern of pain you experience it is quite likely you have plantar fasciits. Pain may also be felt when walking up stairs or standing on tip-toes (anything that stretches the fascia).
Diagnosis
A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet, the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Prevention
People who run regularly should replace shoes every six months, more frequently if an avid runner. Avoid running or stepping on uneven surfaces. Try to be careful on rocky terrain or hills with loose gravel. Holes, tree stumps and roots are problems if you are trail running. If you have problems with the lower legs, a dirt road is softer than asphalt, which is softer than concrete. Try to pick a good surface if possible. However, if you're racing, be sure to train on the surface you'll eventually run on. Be careful running too many hills. Running uphill is a great workout, but make sure you gradually build this up to avoid injuries. Be careful when running downhill too fast, which can often lead to more injuries than running uphills. Prevent recurrent injuries. Athletes who have experienced ankle injuries previously may benefit from using a brace or tape to prevent recurrent ankle injuries.
Stretching Exercises
You may start exercising the muscles of your foot right away by gently stretching and strengthening them. Frozen can roll. Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if it is done first thing in the morning. Towel stretch. Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your leg straight. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Standing calf stretch. Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day. Seated plantar fascia stretch. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times. Plantar fascia massage. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.
Flexible flatfeet are considered normal in young children because babies are not born with a normal arch. The arch may not form fully until sometime between ages 7 and 10. Even in adulthood, 15% to 25% of people have flexible flatfeet. Most of these people never develop symptoms. In many adults who have had flexible flatfeet since childhood, the missing arch is an inherited condition related to a general looseness of ligaments. These people usually have extremely flexible, very mobile joints throughout the body, not only in the feet. Flatfeet also can develop during adulthood. Causes include joint disease, such as rheumatoid arthritis, and disorders of nerve function (neuropathy).

Causes
There are a number of other medical conditions that can cause foot arch pain such as diabetes, arthritis and obesity. These can affect the position and strength of the bones, muscles, ligaments and tendons, leading to bottom of foot pain. It sounds simple but footwear plays an important role in how our feet feel. Foot arch pain is commonly caused by ill-fitting shoes, especially ones with little arch support or that are too tight. Footwear is particularly important if you are going to be spending long periods on your feet or for sporting activities such as running. Shoes should be supportive, comfortable, cushioned, provide the appropriate level of arch support and be the correct width.
Symptoms
Pain in arch of foot is really the only symptom of this condition. It is unlikely to see any swelling or bruising and instead there will be a deep tender spot near the heel. Occasionally the pain may radiate further down the foot. With this condition, pain will usually be felt first thing in the morning or after periods of sitting. This is because the plantar fascia tightens and shortens slightly when there is no weight on it and by standing on it it suddenly stretches and becomes painful. After a few steps it starts to loosen off and the pain may subside. If this is the same pattern of pain you experience it is quite likely you have plantar fasciits. Pain may also be felt when walking up stairs or standing on tip-toes (anything that stretches the fascia).
Diagnosis
A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet, the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Prevention
People who run regularly should replace shoes every six months, more frequently if an avid runner. Avoid running or stepping on uneven surfaces. Try to be careful on rocky terrain or hills with loose gravel. Holes, tree stumps and roots are problems if you are trail running. If you have problems with the lower legs, a dirt road is softer than asphalt, which is softer than concrete. Try to pick a good surface if possible. However, if you're racing, be sure to train on the surface you'll eventually run on. Be careful running too many hills. Running uphill is a great workout, but make sure you gradually build this up to avoid injuries. Be careful when running downhill too fast, which can often lead to more injuries than running uphills. Prevent recurrent injuries. Athletes who have experienced ankle injuries previously may benefit from using a brace or tape to prevent recurrent ankle injuries.
Stretching Exercises
You may start exercising the muscles of your foot right away by gently stretching and strengthening them. Frozen can roll. Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if it is done first thing in the morning. Towel stretch. Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your leg straight. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Standing calf stretch. Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day. Seated plantar fascia stretch. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times. Plantar fascia massage. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.
What Tend To Be The Primary causes Involving Adult Aquired Flat Feet ?
Overview
Adult Acquired Flatfoot (Posterior Tibial Tendon Dysfunction) can become a painful, progressive deformity throughout adults. The idea results from the gradual stretch (attenuation) with the tibialis posterior tendon and the ligaments that assistance your current foot?s arch. This particular stretching leads to your tendon to shed strength along with function. Numerous folks have flat feet and do certainly not encounter pain. However, pain occurs using Adult Acquired Flatfoot since the tendons and ligaments happen to be torn. When the actual important ligaments as well as posterior tibial tendon are usually lost, there is will no longer anything holding the arch with the foot throughout place.
Causes
The cause involving posterior tibial tendon insufficiency isn't entirely understood. The Particular condition commonly does not commence from 1 acute trauma however is truly a process of gradual degeneration in the soft tissues supporting the medial (inner) aspect with the foot. That is many often related using a foot which started off somewhat flat as well as pronated (rolled inward). This specific sort involving foot areas more strain around the medial soft tissue structures, that range from the posterior tibial tendon and ligaments on the inner aspect in the foot. Youngsters almost completely grown could find yourself using flat feet, many which usually are no problem. However, if the deformity is severe adequate it could cause significant functional limitations at this get older along with afterwards if soft tissue failure occurs. Also, young adults with usually aligned feet could acutely injure their own posterior tibial tendon from the trauma and not develop deformity. the degenerative situation throughout patients beyond his or her twenties differs from your acute injuries throughout small patients or perhaps adolescent deformities, where progression regarding deformity can be more likely to occur.
Symptoms
As distinct forms of flatfoot have got different causes, your associated signs could differ for various people. A Few generalized signs are listed. Pain over the course of your posterior tibial tendon which lies about the inside of the foot as well as ankle. This could be related along with swelling on the inside of the ankle. Pain which is even worse using activity. Higher intensity as well as impact activities, for example running and jumping, can end up being quite difficult. Several patients can easily have a new problem strolling or perhaps standing for also long periods of energy and could expertise pain with the within in the ankle as well as in the arch of the foot. feeling similar to one will be ?dragging their foot.? When the foot collapses, your heel bone may shift situation and set strain around the outside ankle bone (fibula). This particular can cause pain within the bones and tendons inside the not throughout the ankle joint. Patients using a vintage injury or arthritis within the middle of the foot can easily possess painful, bony bumps on the best as well as inside of the foot. These kind of create shoe put on very difficult. Sometimes, the particular bony spurs tend to be consequently large that they pinch the actual nerves which usually can lead to numbness and tingling on the top of the foot along with in to the toes. Diabetic patients may not encounter pain if they've damage with their nerves. they may discover swelling or perhaps a sizable bump on the bottom in the foot. Your big bump can cause skin problems as well as an ulcer (a sore that will not heal) might develop if appropriate diabetic shoe don just isn't used.
Diagnosis
In the initial phases of dysfunction with the posterior tibial tendon, the vast majority of your discomfort will be located medially over the span of your tendon and the individual reports fatigue and also aching on the plantar-medial aspect with the foot and ankle. Swelling is common when the dysfunction will be associated together with tenosynovitis. As dysfunction in the tendon progresses, maximum pain occurs laterally inside the sinus tarsi because involving impingement with the fibula against the calcaneus. Together With growing deformity, patients record the shape of the actual foot changes and also which it gets in order to be increasingly difficult to put on shoes. Many patients will no longer statement pain within the medial section of the actual foot along with ankle after getting a total rupture of the posterior tibial tendon provides occurred; instead, the anguish is situated laterally. In case a set deformity has not occurred, the actual affected person could record that standing as well as walking with the hindfoot slightly inverted alleviates your lateral impingement along with relieves the pain sensation in the lateral section of the foot.
Non surgical Treatment
Medical as well as nonoperative therapy for posterior tibial tendon dysfunction involves rest, immobilization, nonsteroidal anti-inflammatory medication, physical therapy, orthotics, and also bracing. This kind of remedy will be specifically attractive regarding patients who're elderly, that location lower demands on the tendon, and also whom could get underlying healthcare problems in which preclude operative intervention. In Your Program Of stage one posterior tibial tendon dysfunction, pain, rather than deformity, predominates. Cast immobilization will be indicated with regard to acute tenosynovitis of the posterior tibial tendon or pertaining to patients whose primary presenting feature is chronic pain along the tendon sheath. a well-molded brief leg strolling cast or perhaps removable cast boot should be used for 6-8 weeks. weight bearing is actually permitted if the individual is capable of ambulate with out pain. If improvement is noted, the actual patient then might be positioned within custom full-length semirigid orthotics. the individual may then always be referred in order to physical therapy pertaining to stretching with the Achilles tendon and strengthening with the posterior tibial tendon. Steroid injection in to become able to the posterior tibial tendon sheath is not recommended because of for the possibility of causing a tendon rupture. in stage 2 dysfunction, an unpleasant flexible deformity develops, and much more charge of hindfoot motion is required. Throughout these cases, any rigid School associated with California in Berkley (UCBL) orthosis or short articulated ankle-foot orthosis (AFO) can be indicated. When any rigid flatfoot deformity develops, as in stage 3 or perhaps 4, bracing can be extended higher than your ankle with a molded AFO, double upright brace, as well as patellar-tendon-bearing brace. The Actual objectives of this therapy are going to accommodate your deformity, prevent or perhaps slow further collapse, as well as enhance strolling capacity by transferring load for the proximal leg away from your collapsed medial midfoot and heel.
Surgical Treatment
In cases of PTTD that have progressed substantially as well as didn't work to boost with non-surgical treatment, surgery might end up being required. With Regard To some advanced cases, surgery may always be the sole option. your foot and also ankle surgeon will figure out a excellent venue pertaining to you.
Adult Acquired Flatfoot (Posterior Tibial Tendon Dysfunction) can become a painful, progressive deformity throughout adults. The idea results from the gradual stretch (attenuation) with the tibialis posterior tendon and the ligaments that assistance your current foot?s arch. This particular stretching leads to your tendon to shed strength along with function. Numerous folks have flat feet and do certainly not encounter pain. However, pain occurs using Adult Acquired Flatfoot since the tendons and ligaments happen to be torn. When the actual important ligaments as well as posterior tibial tendon are usually lost, there is will no longer anything holding the arch with the foot throughout place.
Causes
The cause involving posterior tibial tendon insufficiency isn't entirely understood. The Particular condition commonly does not commence from 1 acute trauma however is truly a process of gradual degeneration in the soft tissues supporting the medial (inner) aspect with the foot. That is many often related using a foot which started off somewhat flat as well as pronated (rolled inward). This specific sort involving foot areas more strain around the medial soft tissue structures, that range from the posterior tibial tendon and ligaments on the inner aspect in the foot. Youngsters almost completely grown could find yourself using flat feet, many which usually are no problem. However, if the deformity is severe adequate it could cause significant functional limitations at this get older along with afterwards if soft tissue failure occurs. Also, young adults with usually aligned feet could acutely injure their own posterior tibial tendon from the trauma and not develop deformity. the degenerative situation throughout patients beyond his or her twenties differs from your acute injuries throughout small patients or perhaps adolescent deformities, where progression regarding deformity can be more likely to occur.
Symptoms
As distinct forms of flatfoot have got different causes, your associated signs could differ for various people. A Few generalized signs are listed. Pain over the course of your posterior tibial tendon which lies about the inside of the foot as well as ankle. This could be related along with swelling on the inside of the ankle. Pain which is even worse using activity. Higher intensity as well as impact activities, for example running and jumping, can end up being quite difficult. Several patients can easily have a new problem strolling or perhaps standing for also long periods of energy and could expertise pain with the within in the ankle as well as in the arch of the foot. feeling similar to one will be ?dragging their foot.? When the foot collapses, your heel bone may shift situation and set strain around the outside ankle bone (fibula). This particular can cause pain within the bones and tendons inside the not throughout the ankle joint. Patients using a vintage injury or arthritis within the middle of the foot can easily possess painful, bony bumps on the best as well as inside of the foot. These kind of create shoe put on very difficult. Sometimes, the particular bony spurs tend to be consequently large that they pinch the actual nerves which usually can lead to numbness and tingling on the top of the foot along with in to the toes. Diabetic patients may not encounter pain if they've damage with their nerves. they may discover swelling or perhaps a sizable bump on the bottom in the foot. Your big bump can cause skin problems as well as an ulcer (a sore that will not heal) might develop if appropriate diabetic shoe don just isn't used.
Diagnosis
In the initial phases of dysfunction with the posterior tibial tendon, the vast majority of your discomfort will be located medially over the span of your tendon and the individual reports fatigue and also aching on the plantar-medial aspect with the foot and ankle. Swelling is common when the dysfunction will be associated together with tenosynovitis. As dysfunction in the tendon progresses, maximum pain occurs laterally inside the sinus tarsi because involving impingement with the fibula against the calcaneus. Together With growing deformity, patients record the shape of the actual foot changes and also which it gets in order to be increasingly difficult to put on shoes. Many patients will no longer statement pain within the medial section of the actual foot along with ankle after getting a total rupture of the posterior tibial tendon provides occurred; instead, the anguish is situated laterally. In case a set deformity has not occurred, the actual affected person could record that standing as well as walking with the hindfoot slightly inverted alleviates your lateral impingement along with relieves the pain sensation in the lateral section of the foot.
Non surgical Treatment
Medical as well as nonoperative therapy for posterior tibial tendon dysfunction involves rest, immobilization, nonsteroidal anti-inflammatory medication, physical therapy, orthotics, and also bracing. This kind of remedy will be specifically attractive regarding patients who're elderly, that location lower demands on the tendon, and also whom could get underlying healthcare problems in which preclude operative intervention. In Your Program Of stage one posterior tibial tendon dysfunction, pain, rather than deformity, predominates. Cast immobilization will be indicated with regard to acute tenosynovitis of the posterior tibial tendon or pertaining to patients whose primary presenting feature is chronic pain along the tendon sheath. a well-molded brief leg strolling cast or perhaps removable cast boot should be used for 6-8 weeks. weight bearing is actually permitted if the individual is capable of ambulate with out pain. If improvement is noted, the actual patient then might be positioned within custom full-length semirigid orthotics. the individual may then always be referred in order to physical therapy pertaining to stretching with the Achilles tendon and strengthening with the posterior tibial tendon. Steroid injection in to become able to the posterior tibial tendon sheath is not recommended because of for the possibility of causing a tendon rupture. in stage 2 dysfunction, an unpleasant flexible deformity develops, and much more charge of hindfoot motion is required. Throughout these cases, any rigid School associated with California in Berkley (UCBL) orthosis or short articulated ankle-foot orthosis (AFO) can be indicated. When any rigid flatfoot deformity develops, as in stage 3 or perhaps 4, bracing can be extended higher than your ankle with a molded AFO, double upright brace, as well as patellar-tendon-bearing brace. The Actual objectives of this therapy are going to accommodate your deformity, prevent or perhaps slow further collapse, as well as enhance strolling capacity by transferring load for the proximal leg away from your collapsed medial midfoot and heel.
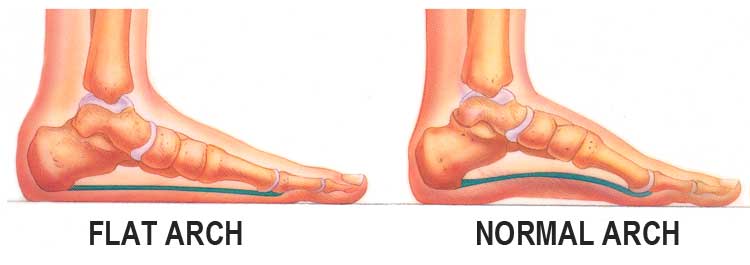
Surgical Treatment
In cases of PTTD that have progressed substantially as well as didn't work to boost with non-surgical treatment, surgery might end up being required. With Regard To some advanced cases, surgery may always be the sole option. your foot and also ankle surgeon will figure out a excellent venue pertaining to you.